Varicose Veins
- Home
- Varicose Veins
Varicose Veins
 Varicose veins are the enlarged tortuous greenish veins seen in the legs and can vary in size from small to huge. Besides being “ugly looking” they can pose a risk to lifestyle (swollen, heavy or painful legs with pigmentation, bleeding or recurrent non-healing wounds) or life (causing blood clots that can break off and go to the lungs). Advances in techniques and equipment have made the treatment less invasive with reduced hospitalisation, convalescence, complications with more comfort and patient friendly outcomes.
Varicose veins are the enlarged tortuous greenish veins seen in the legs and can vary in size from small to huge. Besides being “ugly looking” they can pose a risk to lifestyle (swollen, heavy or painful legs with pigmentation, bleeding or recurrent non-healing wounds) or life (causing blood clots that can break off and go to the lungs). Advances in techniques and equipment have made the treatment less invasive with reduced hospitalisation, convalescence, complications with more comfort and patient friendly outcomes.
What are Veins?
Arteries are blood vessels that carry pure or oxygenated blood from the heart to all parts of the body and Veins are blood vessels that carry impure or deoxygenated blood from all parts of the body back to the heart. Arteries and veins are connected to each other through a system of capillaries that reduces the high pressure from the arterial side to the low pressure on the venous side. Heart pumps blood into the arteries so the flow is always away from the heart and with force that is felt as a pulse. Veins do not have a heart to pump the blood and relies on muscle contraction (foot & calf pump) and provided with uni-direction valves that ensure flow towards the heart and prevent blood flowing back. This is very important in the legs where the flow is against gravity.
What is Varicose veins?
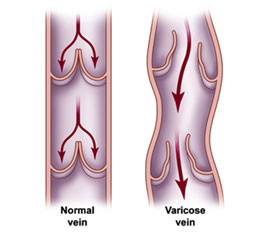 Varicose veins develop when the valves in the veins become defective and cannot prevent blood falling back with gravity in the standing position. This causes stagnation and pooling of blood that results in rise in venous pressure and ballooning of the thin walled veins that become enlarged and tortuous.
Varicose veins develop when the valves in the veins become defective and cannot prevent blood falling back with gravity in the standing position. This causes stagnation and pooling of blood that results in rise in venous pressure and ballooning of the thin walled veins that become enlarged and tortuous.
There are three types of veins in the legs – Superficial: present under the skin and can be seen when enlarged, Deep: present inside the muscle and not seen and perforators: that connect superficial veins to deep veins and are supposed to allow blood to flow in that direction. Varicose veins usually refers to enlargement of superficial veins that become tortuous.
Why do they develop ?
Valves become incompetent due to a family history of weak valves, standing for long periods, overweight and obesity, after pregnancy, advancing age and after damage from blood clots in veins.
What is treatment of Varicose veins?
Treatment involves control of risk factors to prevent recurrence followed by use of limb elevation while sleeping, graduated compression stockings that are more tight near the ankle and less tight as one moves up, exercises and use of venous tonics to increase venous tone. While this form of treatment is very important and helps relieve symptoms and prevents deterioration, it does not help cure veins that have already gone bad.
To get rid of varicose veins treatment options include Ultrasound guided injection foam sclerotherapy offered in isolation for small veins or in combination with endovenous abalation (treatment from inside the vein) using heat generated with either laser (light) or RF (radiofrequency or current). These techniques have revolutionized treatment of varicose veins and only on rare occasions, open surgery (treatment from outside the vein) is used where the superficial vein is disconnected from the deep veins and removed by stripping. Stab avulsions (tiny nicks) with hook phlebectomies are used for removing varicosities.
How does Laser differ from RF abalation?
 Laser uses a temperature of 2000oC to destroy the vein whereas RF uses 120 oC. The heat generated by laser not only destroys the vein but also the fat around the veins. While this is acceptable in large legs it is very ugly and disfiguring in slim ones. The extent of damage is demonstrated in the picture. At times the cutaenous nerve that is located close to the vein also gets damaged and can result in numbness and pain in the legs. Superficial veins can result in skin burns and deep wounds. Hence RF abalation is more gentle and causes less pain, discomfort and complications.
Laser uses a temperature of 2000oC to destroy the vein whereas RF uses 120 oC. The heat generated by laser not only destroys the vein but also the fat around the veins. While this is acceptable in large legs it is very ugly and disfiguring in slim ones. The extent of damage is demonstrated in the picture. At times the cutaenous nerve that is located close to the vein also gets damaged and can result in numbness and pain in the legs. Superficial veins can result in skin burns and deep wounds. Hence RF abalation is more gentle and causes less pain, discomfort and complications.
What is new in RF abalation?
 The RF closurefast “Venefit” is the 3rd generation device that uses a RF catheter with sensor within it that allows the surgeon to know what amount of power is required to destroy the vein. This allows the surgeon to recognize if the vein is completely destroyed or not. He can repeat each 20 second cycle until the machine indicates the vein is destroyed. This reduces the risk of incomplete treatment and residual or recurrent varicose veins. The cost of the catheter is a little more than the Laser fiber but it is money well invested in terms of comfort post procedure and lower risk of nerve and skin injury.
The RF closurefast “Venefit” is the 3rd generation device that uses a RF catheter with sensor within it that allows the surgeon to know what amount of power is required to destroy the vein. This allows the surgeon to recognize if the vein is completely destroyed or not. He can repeat each 20 second cycle until the machine indicates the vein is destroyed. This reduces the risk of incomplete treatment and residual or recurrent varicose veins. The cost of the catheter is a little more than the Laser fiber but it is money well invested in terms of comfort post procedure and lower risk of nerve and skin injury.
What is new in anesthesia?

 Endovenous abalation can be performed under local anesthesia using a technique called “Tumescent Anesthesia”. This involves injection a mixture of cold saline mixed with local anesthetic all around the vein after the catheter is in place that ensures that the procedure of destroying the vein is painless, causes the enlarged vein to go into spasm and maintain contact with the catheter ensuring complete damage of the wall and separates the skin and nerve from the adjacent vein thereby protecting it from damage. Using a Tumescent pump ensures lesser number of needle pricks, better infiltration and reduces time required for the surgery. Patients can choose to get the procedure done as a day care or with admission depending on their preference.
Endovenous abalation can be performed under local anesthesia using a technique called “Tumescent Anesthesia”. This involves injection a mixture of cold saline mixed with local anesthetic all around the vein after the catheter is in place that ensures that the procedure of destroying the vein is painless, causes the enlarged vein to go into spasm and maintain contact with the catheter ensuring complete damage of the wall and separates the skin and nerve from the adjacent vein thereby protecting it from damage. Using a Tumescent pump ensures lesser number of needle pricks, better infiltration and reduces time required for the surgery. Patients can choose to get the procedure done as a day care or with admission depending on their preference.
What is the latest in treatment of Varicose veins?
 The above complication can be avoided by treating the varicose veins with modern glue therapy using n-butyl-2-cyanoacrilat (NBCA) – a medical super-glue that is approved by the US FDA. The formulation used to treat varicose veins is called Venaseal and is more viscous as compared to other medical super glues available and has less change of slipping out and escaping into the normal veins from the target site. This is a type of non-thermal non-tumescent treatment for varicose veins.
The above complication can be avoided by treating the varicose veins with modern glue therapy using n-butyl-2-cyanoacrilat (NBCA) – a medical super-glue that is approved by the US FDA. The formulation used to treat varicose veins is called Venaseal and is more viscous as compared to other medical super glues available and has less change of slipping out and escaping into the normal veins from the target site. This is a type of non-thermal non-tumescent treatment for varicose veins.



