Carotid Arterial Disease
- Home
- Carotid Arterial Disease
Carotid Arterial Disease
Introduction

The brain is supplied by two arteries on each side – one in the front of the neck is called “Carotid artery“ and one at the back near the vertebrae is called “Vertebral artery”. The four arteries (two from each side) meet each other in the brain in an area called the “Circle of Willis”.
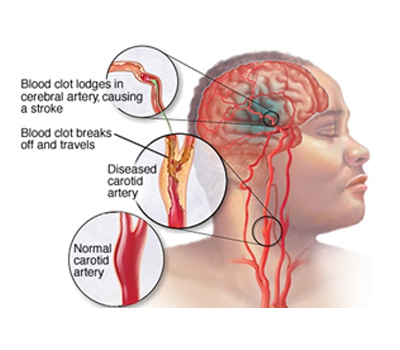
When these arteries get diseased due to deposition of plaques, the blood supply gets reduced but if only one artery is diseased, the other arteries can compensate for the reduced flow unless the plaque or blood clot from the roughened inner surface breaks and flies off and blocks the smaller arteries when it may result in damage to the brain cells. If more than one artery is blocked then body compensates by raising the blood pressure and whenever the blood pressure drops there is reduced blood supply (hypoperfusion) and patient tends to lose consciousness, falls down so that blood supply is restored by eliminating gravity and increasing flow from the legs that are no longer erect.
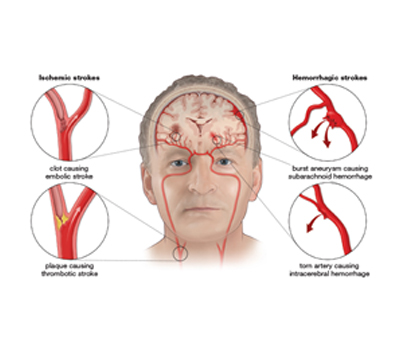
Damage to the brain or stroke can occur either due to reduced blood flow (Ischemic stroke) or due to bleeding into the brain due to rupture of the artery (Hemorrhagic stroke) that takes place when there is ballooning or aneurysm of the artery.
We will be focusing on ischemic stroke that often arises due to disease of the carotid artery.
Cause
Carotid arterial disease results due to high blood pressure, diabetes, high cholesterol, smoking. In rare cases it may also arise due to inflammation (Vasculitis or Arteritis).
Symptoms
In most cases the narrowing may be asymptomatic and chances of symptoms occurring depend on degree of narrowing (> 70%) and involvement of >1 artery. Symptoms produced can vary depending on area of the brain compromised. Usually before a major stroke occurs there are >1episodes of a minor stroke or TIA that recovers within a few minutes. The symptoms may present as:
- Transient loss of consciousness (hypoperfusion) or
- Weakness involving one upper or lower limb (monoplegia or paresis) or both (hemiplegia or paresis) involving one side of the body (side opposite to the diseased artery).
- Slurring of speech (dysarthria) that is more common with left carotid in right handed individuals or facial asymmetry with drooling of saliva.
- Blurring of vision called Amaurosis Fugax or loss of vision (emboli to Opthalmic artery on same side of the diseased carotid).
- Loss of vision in some parts of the visual field (damage to back part of the brain – occipital lobe).
- Imbalance when getting up (Vertebro-basilar) TIA.
If the brain cells get ischemic or damaged (infarct) the weakness may recover early and completely within a few seconds to minutes to hours (TIA). Recovery may either be partial with mild to moderate deficit or may not recover at all (Stroke).
Diagnosis
 It is a usual practice that as part of vascular examination the doctor puts his stethoscope on the carotid artery in the neck. If it is narrowed one may be able to hear a whooshing sound called a “Carotid bruit” & indicates the presence of arterial narrowing.
It is a usual practice that as part of vascular examination the doctor puts his stethoscope on the carotid artery in the neck. If it is narrowed one may be able to hear a whooshing sound called a “Carotid bruit” & indicates the presence of arterial narrowing.
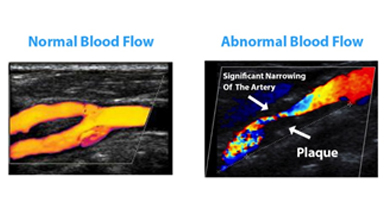 This is further investigated by performing a Carotid Doppler Sonography where all 4 vessels are examined, extent and degree of narrowing identified along with nature of the plaque, presence of thrombus.
This is further investigated by performing a Carotid Doppler Sonography where all 4 vessels are examined, extent and degree of narrowing identified along with nature of the plaque, presence of thrombus.
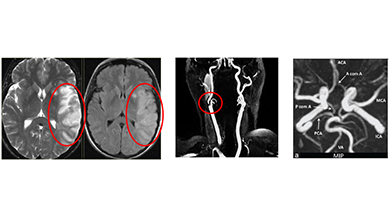 It is customary to also ask for MRI of the brain to look for areas of damage (infarct) along with MR angiography to look at all the 4 vessels in the neck and inside the skull including the formation of the Circle of Willis.
It is customary to also ask for MRI of the brain to look for areas of damage (infarct) along with MR angiography to look at all the 4 vessels in the neck and inside the skull including the formation of the Circle of Willis.
 Prior to intervention it is customary to get either an CT angiography or a Digital Subtraction Angiogram (DSA) done to look at the location and extent of the disease segment as well as the collateral circulation in the brain.
Prior to intervention it is customary to get either an CT angiography or a Digital Subtraction Angiogram (DSA) done to look at the location and extent of the disease segment as well as the collateral circulation in the brain.
Besides these imaging studies, one also evaluates the risk factors (through blood tests) and the condition of the heart (2D echo) to rule out cardiac source of clots as well as identify if the heart is strong enough (Dobutamine Stress Echo or Stress Thallium scan) for open surgical or endovascular intervention.
Treatment
Medication is immediately started to thin the blood, improve circulation to the brain and control risk factors. High dose of anti-cholesterol drugs (statins) is also given to stabilize the plaque.
Decision then needs to be taken regarding choice and timing of intervention.
Choice of intervention includes either open surgery called “Carotid Endarterectomy” where the artery is cleaned of the diseased portion and then closed directly or with a patch (vein or synthetic – Dacron or PTFE) to increase the size of the artery or Endovascular procedure called “Carotid Angioplasty and Stenting”.

The choice of procedure depends on the location and extent of the disease segment, presence of clots and cardiac risk.
Timing of surgery depends on extent of damage (infarct) in the brain due to the current episode as well as the severity of the narrowing. If the area of damage is small, one performs the procedure at the earliest. If the area is large, one waits for 4 weeks for the area to heal unless the disease is so severe that there is a risk of another stroke during the waiting period.
It is known (NASCET and ECST trial) that when the narrowing exceeds 70% and there are symptoms the risk of another stroke is almost 27% within 2 years if treated only with medicines and the risk reduces to 9% if treated surgically.
It there are no symptoms and the narrowing is > 80% then the risk of a stroke within 2 years is 10% if treated only with medicines as against 5% if treated surgically (ACAS Trial).
Choice between open surgery and Angioplasty-stenting depends on location, extent of disease with amount of calcification, age of the patient and risk factors that influence decision making. Both procedures give good results in symptomatic and asymptomatic carotids if the patient selection is done properly.


